Evisceration for endophthalmitis
The treatment of endophthalmitis in a no-light perception eye is controversial. If the infection and pain are under control and the retina doctor has done all they can do, then observation is an option. The eye will probably become phthisical (shrunken). If the infection is not under control or if the patient is having uncontrollable pain, then an evisceration or enucleation should be performed. Classic teaching recommends evisceration for fear of causing a deeper infection with an enucleation. With current antibiotics, most of us believe that an enucleation can be performed safely. I prefer an evisceration for endophthalmitis. The second question is whether or not to place an orbital implant. I believe the risk of infection is low when placing a concurrent implant, therefore I do place one.
For a written transcript of this video, please see below:
This is Richard Allen at the University of Iowa.
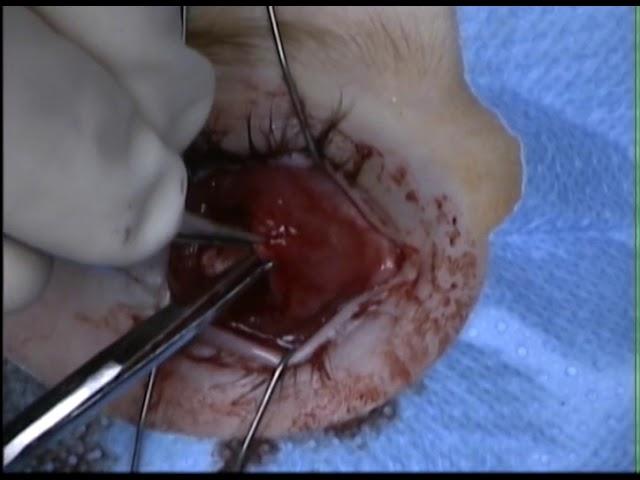
This video demonstrates an evisceration in a patient with endophthalmitis.
Due to the significant inflammation in this case and tendency for bleeding due to the inflammation, a retrobulbar block and subconjunctival injection are placed with lidocaine and bupivacaine with epinephrine. The Westcott scissors are used to perform a 360 degree peritemy. There is often a bit of oozing, which in general can be ignored as it will stop. A supersharp blade is then used to make incision through the sclera at the posterior limbus. Westcott scissors are used to complete a 360 degree incision at the posterior limbus. This can be performed with Castro-Viejo scissors if preferred. The purulent material from the endophthalmitis is noted. An evisceration spoon is then introduced into the suprachoroidal space and the contents of the eye with the cornea attached are removed and sent to the pathologist for evaluation. Again, due to the significant inflammation, there can be a bit of bleeding from inside the scleral shell. Cotton tipped applicators soaked in absolute alcohol are used to denature any remaining uvea in the scleral shell. The shell is then irrigated with saline. The posterior sclera is then incised with the 15 blade. Utility scissors are used to enlarge the incision across the back of the shell. The optic nerve is palpated and cut. The end of the optic nerve attached to the shell is then identified and excised. This is sent to the pathologist to evaluate for any spread of the infection in the space between the optic nerve and optic nerve sheath.
The anterior sclera is then incised so that an implant can be placed. The intraconal space posterior to the posterior sclera is demonstrated. The placement of the implant was not captured on this video, unfortunately. Usually I prefer an 18 or 20 mm PMMA implant.
The posterior sclera is then closed over the implant with interrupted 4-0 Vicryl sutures. The anterior sclera is then closed by imbricating the sclera over itself. In this case, the inferior sclera is imbricated over the superior sclera. This is performed with a running mattress suture so that the two edges are imbricated over each other. This results in two layers of sclera over the implant. The conjunctiva is then closed over the sclera to provide a third layer over the implant. I do not feel that closure of Tenon’s is necessary with two layers of sclera and a layer of conjunctiva.
A conformer is placed. Due to the fact that there will be a bit of inflammation after this surgery, a temporary suture tarsorrhaphy is placed. This is performed with 5-0 chromic suture. These sutures will usually dissolve by about three weeks. An eye pad is placed and the patient will return in one week.
Over 300 oculoplastic surgery videos are available, free of charge, at http://www.oculosurg.com
For a written transcript of this video, please see below:
This is Richard Allen at the University of Iowa.
This video demonstrates an evisceration in a patient with endophthalmitis.
Due to the significant inflammation in this case and tendency for bleeding due to the inflammation, a retrobulbar block and subconjunctival injection are placed with lidocaine and bupivacaine with epinephrine. The Westcott scissors are used to perform a 360 degree peritemy. There is often a bit of oozing, which in general can be ignored as it will stop. A supersharp blade is then used to make incision through the sclera at the posterior limbus. Westcott scissors are used to complete a 360 degree incision at the posterior limbus. This can be performed with Castro-Viejo scissors if preferred. The purulent material from the endophthalmitis is noted. An evisceration spoon is then introduced into the suprachoroidal space and the contents of the eye with the cornea attached are removed and sent to the pathologist for evaluation. Again, due to the significant inflammation, there can be a bit of bleeding from inside the scleral shell. Cotton tipped applicators soaked in absolute alcohol are used to denature any remaining uvea in the scleral shell. The shell is then irrigated with saline. The posterior sclera is then incised with the 15 blade. Utility scissors are used to enlarge the incision across the back of the shell. The optic nerve is palpated and cut. The end of the optic nerve attached to the shell is then identified and excised. This is sent to the pathologist to evaluate for any spread of the infection in the space between the optic nerve and optic nerve sheath.
The anterior sclera is then incised so that an implant can be placed. The intraconal space posterior to the posterior sclera is demonstrated. The placement of the implant was not captured on this video, unfortunately. Usually I prefer an 18 or 20 mm PMMA implant.
The posterior sclera is then closed over the implant with interrupted 4-0 Vicryl sutures. The anterior sclera is then closed by imbricating the sclera over itself. In this case, the inferior sclera is imbricated over the superior sclera. This is performed with a running mattress suture so that the two edges are imbricated over each other. This results in two layers of sclera over the implant. The conjunctiva is then closed over the sclera to provide a third layer over the implant. I do not feel that closure of Tenon’s is necessary with two layers of sclera and a layer of conjunctiva.
A conformer is placed. Due to the fact that there will be a bit of inflammation after this surgery, a temporary suture tarsorrhaphy is placed. This is performed with 5-0 chromic suture. These sutures will usually dissolve by about three weeks. An eye pad is placed and the patient will return in one week.
Over 300 oculoplastic surgery videos are available, free of charge, at http://www.oculosurg.com
Тэги:
#ophthalmology #oculoplastic #oculoplastics #oculofacial #eye_surgery #evisceration #endophthalmitisКомментарии:
Evisceration for endophthalmitis
Richard C. Allen MD PhD FACS
Robbing Beehives | Minecraft anime
실패자_silpaeja
Kenny Rogers - Lucille (Audio)
Kenny Rogers
My everyday makeup using local products | Stephanie Concepcion
Stephanie Concepcion
Latest Ten Collection of Surprises
Ibibna Review
Infinite Curiosity
Thetahealing - Topic
now I show you some trick or two
afrosmaximus
The Pharox LED Bulb on The Early Show
Dledlight
ChromaLight's Cyclorama Green Chroma Key Paint | NAB 2024
CUE-Support B.V.